
Urological disease
Prostate cancer
• What is the prostate for?
The prostate is a gland situated below the bladder in front of the rectum. It is useful for the production of semen and so essential to reproduction. In adulthood it reaches the size of a chestnut.
The urethra, a canal which evacuates the urine, passes through the prostate. So when the prostate swells, it can disturb/interfere with urination/ cause troubles with urination/ can cause problems to urination.
• • • • • •
• What is prostate cancer ?
With more than 40 000 new cases per year, prostate cancer is the first most frequent cancer in France, before lung cancer. One man out of nine will develop some form of clinical prostate cancer in his lifetime, with an average age for the diagnosis generally between 60 and 90.
This cancer is due to the anarchic growth of prostate cells which have shifted away from their original function and can spread to others organs (metastases).
• • • • • •
• What are the symptoms of prostate cancer ?
In the early stages of a local prostate cancer there are no clinical signs. Blood in urine, pains, troubles to urinate and a weakening of general health appear most often when the cancer has become more aggressive and has already spread beyond the prostate gland. Screening is therefore advised to detect the tumours when they are still confined to the prostate gland.
• • • • • •
• How to detect prostate cancer ?
The French Urology Association recommends a yearly digital rectal examination ( DRE) and test to check the level of PSA in blood for men aged between 50 and 75, and as early as 45 years old for men with a family history or an ethnic risk. With a DRE, any irregularity will be felt as this cancer usually spreads in the peripheral area of the prostate.
PSA (Prostate Specific Antigen) is a biological marker produced by the prostate only which shows the gland activity. A rise in the level of PSA in the blood can identify patients at risk of prostrate cancer but this rise can also be caused by other troubles like infection, size of the gland or prostatic massage.
Prostate endorectal biopsies are the only current mean to prove/confirm with certainty the presence of prostate cancer. It is performed transrectally using a thin needle under ultrasound guidance after the patient has taken an antibiotic and stopped any blood thinning treatment.
• • • • • •
• How to treat prostate cancer ?
Since the evolution of a prostate cancer is often very slow even with no treatment and as a number of these tumours can remain silent for a whole life, the choices of treatment strategies offered are modulated according to life expectancy. When the cancer is localised, an appropriate treatment can eradicate the disease.
Surgery : A radical prostatectomy is a procedure which removes the entire prostate gland. This procedure is offered in the first instance to the youngest patients. This operation can now be carried out by laparoscopy with a robot monitored by the surgeon ( Da Vinci Robot ). The aim is to promote a better quality of dissection / incision and a "minimally invasive" approach. The possible troubles after such surgery are erectile dysfunction and urinary incontinence.
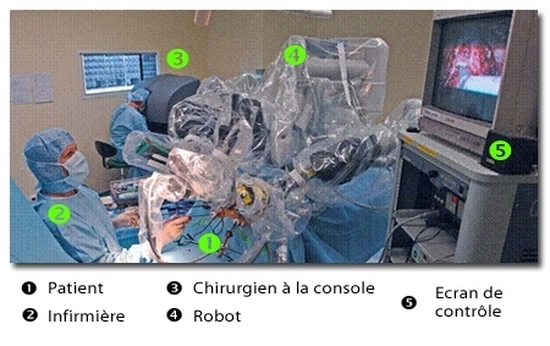
"Robotic Surgery"
Radiotherapy : Irradiation of the gland with radiation therapy aims to destroy the prostate tumour. The treatment lasts on average seven weeks and its complications are mainly digestive and urinary irritations and to a smaller extent erectile dysfunction and urinary incontinence.
Brachytherapy : In this treatment, radioactive iodine pellets are implanted in the prostate in a single operation carried out under general anaesthetics.
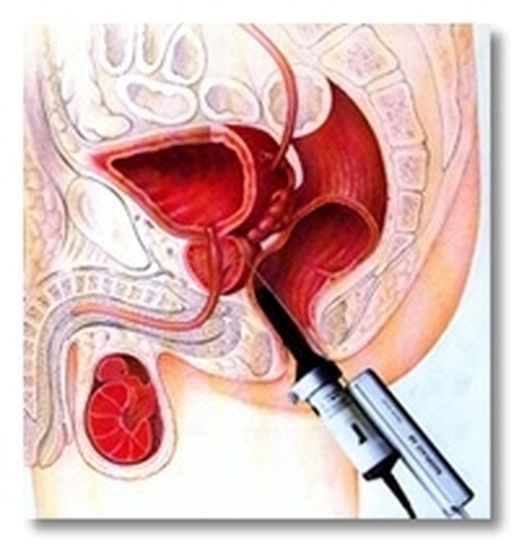
High Intensity Focused Ultrasound (HIFU) :
This method is being evaluated. It delivers into the prostrate gland a beam of high intensity focused ultrasound via an endo-rectal probe under general anaesthetics once the size of the prostrate has been reduced via an endoscopic transurethral resection ( TURP = transurethral resection of the prostrate).
When the cancer is more advanced the previous treatments are not enough and often hormonal therapy, which acts as a chemical castration, is given to block the rate of cancer growth.
• • • • • •
Urinary incontinence and prolapse
• Pelvic Organs Prolapses in women
Everyone knows about the diaphragm (a sheet of muscle extending across the bottom of the rib cage and crucial in breathing and respiration) but did you know that there is also a muscular "diaphragm", across the bottom of your pelvis which maintains your pelvic organs (bladder, vagina, uterus, rectum) in place when standing up?
When this floor sags, the organs gradually "cast off their mooring" and slip/slide downwards until they appear like lumps of varying sizes through the vagina.

MRI push prolapse
Why this lapse ?
The main causes are lower muscular resistance due to old age, the stretching of muscles and ligaments during childbirth, lack of hormones.
What are the symptoms ?
At the beginning you may experience a feeling of heaviness or slight pain in the pelvic area when standing up for a long time. Then a small lump appears which can fall further than the vulva but which goes back in again when lying down. Constipation is frequent as well as uneasy or painful intercourse. On the other hand, urinary incontinence is rare.
Further examination
A simple medical examination in the gynaecological posture can already establish a precise diagnosis. It will be completed, amongst others, by an ultrasound and sometimes and MRI (Magnetic Resonance Imaging).
Treatment
A surgical procedure can be an option if the prolapse is important and causes unease as soon as you stand up. Carried out via laparoscopy, it fixes the organs definitely with polypropylene mesh (promotofixation).
Other techniques may be used, depending on the cases.
The main thing is to find the best possible comfort for the three functions : urinating, intercourse, bowel transit.
• • • • • •
• Urinary Incontinence
We are talking here of urine leaking through the urethra outside of urination. These leaks can happen when you are making an effort like coughing, dancing, carrying something, walking down a footpath, getting up... (stress incontinence) or can manifest themselves as an urgent need which cannot be repressed / controlled (urge incontinence).
These two situations must be clearly identified as they correspond to different mechanisms and treatments. Stress incontinence can benefit from surgery (the now well-known mesh bands). Urge incontinence is more clinical. On the whole, the unease is variable and is considered important if the patient has to wear pads.
What should you do when you feel you are loosing your bladder control ?
First of all do not be afraid to talk to your doctor, your gynaecologist, your friends. Then find a specialist who will make a diagnosis by asking questions and examining you. A special examination, the urodynamic testing, is often done in addition.
The choice between surgery, re-education, or medication will ,as always, be made following a specific and precise diagnosis.
• • • • • •
Urinary lithiasis
Urine is produced by the kidneys and flow through tubes, the ureters, into the bladder, a reservoir which empties itself through the urethra. Stones, the "calculi", can form anywhere within this system which constitute the urinary tract. Their medical name is "renal lithiasis".
The vast majority of kidney-stones are spontaneously eliminated but some may need to be treated as they can get stuck in the cavities and tubes and cause a blockage. This manifests itself in various way , in particular severe pains, called renal colic.
• What are the treatment ?
Extracorporeal shock wave lithotripsy (ESWL) is one of the treatments. It is the breaking-up of a kidney-stone via shock waves sent by a machine, without any surgery procedure, the patient simply lying down on a table. The fragments are then eliminated in a natural way in the days following the treatment.
If the treatment should fail or if it is impossible to apply such treatment, a surgery procedure may be carried out in hospital under general anaesthetics. Various types of surgery are available:
- The ureteroscopic stone removal is an endoscopic procedure. Under videoscopy the surgeon will pass through the urethra and bladder a small tubular instrument, the ureteroscope (also called cystoscope), to reach the kidney-stone. The stone can then either be removed (using an instrument with a "basket" attachment ) or fragmented with the help of a lithotripsy instrument (mechanical, ultrasound, hydroelectric or laser ) brought into contact with it.
- The percutaneous nephrolithotomy (PCNL) : is a kidney puncture through the skin after a the creation of an access tunnel and a port placement to introduce into the kidney the extracting or fragmenting instruments
- Finally, the treatment of a kidney stone may need the more conventional approach of an open surgery procedure, where the incision is done in the usual way or in centres specialised in key hole surgery (laparoscopy) whereby very tiny incisions are made.
• What must you do in case of a severe painful crisis ?
First do not panic even though renal colic pain is known to be one of the most severe pain with no relief position. Drink less, go to emergency, have a simple x-ray (ASP and ultrasound). Very often an anti-inflammatory and anti-spasmodic treatment is enough to ease the crisis. A scan done in the emergency ward can sometimes help the diagnosis in doubtful cases. Hospitalisation is advised if there is a fever, a single kidney or unbearable pains which cannot be eased.
When there are severe pains or complications due to the kidney-stone, it may be necessary to place a JJ stent ( so called because of its curved shape at each end) between the bladder and the kidney to evacuate the urine.
• Prevention of kidney stones ?
This will depend on the chemical nature of the kidney stone once it has been analysed. For example, with uric acid stones you will have to follow a specific diet and a treatment (alkalinization) to reduce acid in the urine. Some calcium oxalate stones may be caused by a serious condition called hyperparathyroid. A blood test will be prescribed in case of lithiasis.
• What can bring about urinary lithiasis ?
Anything that leads to a stagnation of urine in the "pipes" : kidney and ureter malformation, prolonged confinement, pregnancy, dehydration, etc… « Metabolic » causes depend on blood and urine composition and are complex. There can sometimes be an hereditary aspect .
• • • • • •
Infertility
• When to consult ?
When a couple is thinking about having a child, they do not know if they are fertile or not. It is usually only after a few months of not achieving conception that the decision to consult is taken. It is in fact unnecessary to worry too early. The natural delay to conceive is on average 5 to 6 months in France. It is no use consulting before then. On the other hand, if conception does not occur after two years of unsuccessful attempts, the usefulness of medically assisted conception has been proven.
About 10 percent of couples are faced with a fertility problem. Among these, it is a male problem in one out of two cases. Therefore if the first consultation is at the gynaecologist, a male check up is very often necessary.
• • • • • •
• What treatment ?
The first examinations to sort out the different causes are temperature graph for woman, post-coital Hunher test for the couple, and a semen analysis (spermogramm and spermocytogramm) for the man. These simple examinations can be prescribed by your GP or your gynaecologist. When the sperm test shows an abnormality, a urologist (qualified in andrology) will take over and will carry out a detailed examination of the genital system (testes, canals, prostrate, seminal junction) with an ultrasound if necessary.
The medically assisted conception team has been officially accredited by the ministry.

The urologist cooperate with the whole team :
- The biologist who carries out, if necessary, more detailed evaluations of levels in blood and sperm. Micromanipulation of gametes ( spermatozoids and ovocytes) and embryos as well as semen and embryo freezing (cryopreservation) can be done too.
- The gynaecologist may recommend artificial insemination (AI) or in vitro fertilisation (IVF).
Sometimes to treat the cause of infertility in man requires surgery: if there is a varicocele, obstructing the canals, the spermatozoids are directly collected in the testicle via a tiny incision. This surgery procedure is carried out by a urologist under a general anaesthesia and you will need to stay in hospital for up to three days.
The majority of couples who undergo a medically assisted reproductive treatment are able to conceive. True sterility is rare. In all cases a detailed diagnosis and a precise prognostic are available.
• • • • • •
